What is the best treatment for sciatica?
An explanation of nerve pain in the leg and how it can be treated
What is sciatica?
Both our Falkirk and Perth teams see many patients with sciatica. Sciatica is pain that goes down the leg from the lower back. The pain may be located on the outside, back, or front of the leg. It often manifests as a tight, gripping pain in the buttock, which may move up to the base of the back or down into the leg. It may stop above the knee or go down all the way to the foot and toes. Occasionally it can also travel around to the groin area. Usually it is found only on one side of the body, but occasionally both legs are affected. Sometimes there is pain in the low back in conjunction with sciatica, but not always. Classic sciatica feels like a “nervy” pain, but numbness / tingling or weakness of the leg, foot, and toes may also be present. The pain usually feels shooting, stabbing, gripping, or burning (as if the leg is on fire).
Sciatica may vary in intensity. Sometimes it may be just an annoying niggle. It may stop people from engaging in activities that they used to enjoy, such as gardening, walking the dog, or playing with their children. Or it may be crippling you to the point where they cannot walk, cannot work, and are at their wits’ end.

treat sciatica pain
What is the sciatic nerve?
The sciatic nerve is formed by several spinal nerves which exit the spinal cord around the lower lumbar vertebrae and the sacrum (L4 to S3). These nerve branches unite and form the sciatic nerve, which travels goes behind the hip joint, down the buttock, and down the back of the leg into the foot. It is the longest and thickest nerve in the human body – it is about as thick as a pencil! It provides sensation to almost the entire skin area of the leg and foot, and gives power to the muscles located at the back of the thigh, and those of the lower leg and foot. Behind the knee, the sciatic nerve divides into two smaller branches which supply the back of the lower leg and foot and the front and side of the lower leg, respectively.
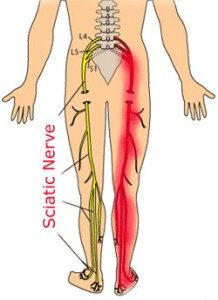
Sciatic Nerve
What causes sciatica?
Sciatica is caused when the sciatic nerve or its branches get irritated. Most commonly, this happens where the different nerve branches exit the spinal cord, i.e. in the low back or around the sacrum. Sometimes it happens behind the knee, where the sciatic nerve splits into two branches. Neurosurgeon Alf Breig spent the 1950s to 1980s researching how the nervous system works [1]. He discovered that a nerve starts to function differently if it gets stretched. Once the stretch is removed, the nerve starts to work again. In previous blogs post we discussed how the spinal cord functions. We described in some detail how misalignments in the spine can have a negative effect on how the nerves in the spinal cord work and how this can cause symptoms such as pain, tingling, numbness, or weakness.
Most of the time, problems with nerves are related to the nerve getting stretched because there is a mechanical distortion happening somewhere in the body (most likely a misaligned spine). This is easy to address and correct. The exceptions are problems directly related to cancer, infection, diabetes, or damage to the nerve caused by accidents, fractures, or surgery. These follow different rules, and sometimes it is not possible to repair the damage.
Let’s look at how this applies to the sciatic nerve
Misalignments in the low back or pelvis (sacrum), or even in the knee, can stretch the sciatic nerve (or its branches) in various areas. Any nerve is made up of a variety of different fibres: some report pain back to the brain; some are responsible for controlling muscle function and therefore movement and strength; others provide the brain with information about what is happening to the body part – is it getting scratched, pinched, or touched lightly? Is it hot or cold? And what is its position in space, related to gravity? As a nerve gets stretched, one or more types of nerve fibres can get affected. Depending on which ones get impacted, different symptoms may show up: pain, weakness, burning, tingling, numbness, a “dead” feeling in the limb, hypersensitivity or decreased sensation.
How is sciatica diagnosed? How can it be treated?
Sciatica is diagnosed primarily by taking a detailed history. We will ask you many questions about where the pain is located, what it feels like, how intense it is. We want to know when you are feeling it — is it constant? Does it come and go with certain activities or at certain times of the day? Did you have an accident or surgery? Did you ever have a serious illness such as cancer? Did you ever break any bones? All of this gives us information so we can work out what’s going on with your pain and where it is coming from. We will also examine your back and legs. Different tests will tell us what is going on.
Scientists in Finland did a study of 2,946 women and 2,727 men (age range, 30-64 years) who suffered from back problems [2]. Those with a previous traumatic back injury had a 2.5-fold risk of having sciatica or low back pain. This is why we are interested not only in recent accidents or surgeries. We want to know everything that has happened to the structure of your body since childhood, as it can take years for problems to build up to the point where things hurt!
Sometimes patients who have sciatica get an MRI or X-ray taken. This very likely shows problems in the low back area: degeneration of the bones and joints, “wear and tear”, or disc problems. All of these are a direct result of a misaligned spine which creates mechanical distortion. This, in turn, leads to the stretching of the nerves as described above. The previous idea of a “pinched” nerve is rather outdated by now, even though doctors might still call it that. The real problem is the stretching of the nerves as they have to follow the misalignments of the bones. MRIs show the nerve getting thinner – but think of a rubber band getting stretched: it gets thinner as it gets stretched more and more. “Pinching” is not the problem, stretching is.
Sometimes doctors recommend surgery for sciatica. However, studies show that most of the time these surgeries are not successful. While they provide rapid pain relief in the first three months, patients are often left with mild to moderate pain five years after the surgery. [3]
With Advanced BioStructural Correction™, we address the root cause of sciatica. We correct the underlying structural misalignments of the spine. This improves and restores joint function and mobility. More importantly, it greatly reduces the stretching of the nerves. Once we get to the bottom of the problem, the sciatica pain and other symptoms related to it will go away. We will also offer advice about certain lifestyle modifications to help you prevent any additional stretching of the nerves by, for example, sitting the wrong way. This will ensure that our patients do not inadvertently cause any setbacks to their progress on the journey towards getting out of pain.
If you are experiencing pain or other symptoms in your legs, give us a ring and book in for a free consultation to see how we can help. When you come in, have a chat with our receptionist, Rachel. She suffered greatly from sciatica, but Advanced BioStructural Correction™ gave her back her life so she can move without pain and enjoy time with her children. Here’s what Rachel says:
“I felt like I was in my 70s when I was in my 40s. The pain stopped me enjoying my children. I had to roll out of bed in the morning. Now the pain is almost gone after a couple months of treatment.”
- Breig, Alf. Adverse Mechanical Tension in the Central Nervous System: An Analysis of Cause and Effect. Almqvuist & Wiksell International, Stockholm, Sweden, 1978.
- Heliövaara M1, Mäkelä M, Knekt P, Impivaara O, Aromaa A. Determinants of Sciatica and Low-Back Pain. Spine (Phila PA 1976). 1991 Jun;16(6):608-14. https://www.ncbi.nlm.nih.gov/pubmed/1830689.
- Machado GC1, Witzleb AJ1, Fritsch C2, Maher CG1, Ferreira PH3, Ferreira ML. Patients with Sciatica still Experience Pain and Disability 5 Years after Surgery: A Systematic Review with Meta-Analysis of Cohort Studies. Eur J Pain. 2016 May 12. doi: 10.1002/ejp.893. [Epub ahead of print]. https://www.ncbi.nlm.nih.gov/pubmed/27172245.
Image source:
https://www.painscience.com/imgs/sciatica-avatar-m.jpg
https://uk.pinterest.com/joanharvey/health



